INTEGRATING HEALTH LITERACY IN EXPERIENTIAL LEARNING
Shirish Lala, EdD(c), MHS, OTR/L Academic Fieldwork Coordinator Daytona State College
The pursuit of acquiring literacy is intentional, purposeful, and deictic, and subject to change based on the contextual demands (Leu, Kinzer, Coiro, Castek, & Henry, 2013). Literacy can be loosely defined as a construct that provides an individual with the ability to read, write, and integrate information across a broad range of platforms in order to identify, recognize, and implement knowledge for the purpose of personal,social, or financial gain. The U.S. Department of Health and Human Services describes health literacy (HL) as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (National Network of Libraries of Medicine [NNLM], 2011). However, according to the Centers for Disease Control, low HL is a serious public health issue affecting nine out of every ten adults (Centers for Disease Control [CDC], 2018a). At least 50% of the adults without high school education are at risk for experiencing severe health crises including medication errors, increased hospital visits, higher mortality, and greater health expenditure as compared to those with adequate HL levels (Brach et al., 2012).
Low literacy statistics are even more staggering in geriatric populations in which over 70% of older adults are reported to experience difficulties with using print materials and electronic health media (CDC, 2018b). In addition, health professionals frequently overestimate HL abilities in ethnic minorities, low-income groups, and immigrant client populations (Weekes & Phillips, 2015). Poor health care outcomes due to low HL rates in sensitive population groups costs the U.S. economy about $106 billion to $238 billion annually, which is why the CDC recommends all educational settings take incremental steps in incorporating standard-based curriculum with developmentally appropriate health and science information to increase awareness about health literacy (CDC, 2018a; Vernon, Trujillo, Rosenbaum, & DeBuono, 2007). This article will discuss the rationale for implementing health literacy into the curriculum of occupational therapy assistant (OTA) programs, as well as explicitly linking it with experiential education opportunities.
Legislation, like the Patient Protection and Affordable Care Act, emphasizes the importance of health literacy when delivering high-quality healthcare at subsidized costs. The goal of promoting health literacy within OTA curriculum is supported by educational standard B.4.21 published by the Accreditation Council for Occupational Therapy Education, which states prior to graduation an OTA student must successfully “demonstrate the principles of the teaching-learning process using educational methods and health literacy approaches” (Accreditation Council for Occupational Therapy Education [ACOTE], 2018, p. 31). Since Daytona State College primarily serves the residents of Volusia and Flagler county, which houses one of the largest concentrations of older adults in the state of Florida, the OTA program is in the process of organizing resources to enhance stakeholders’ awareness of health literacy across practice settings Importance of Health Literacy in the Occupational Therapy Assistant (OTA) Curriculum Shirish Lala, EdD(c), MHS, OTR/L Academic Fieldwork Coordinator Daytona State College FLOTEC Mission Statement: To promote, encourage, and foster quality fieldwork education in collaboration with fieldwork educators for the benefit of all Occupational Therapy students in the state of Florida. (ACOTE, 2018; Gant, 2013).
Stakeholders include students, practitioners, fieldwork educators, and others involved in fieldwork training. The assessment of a senior patient’s HL is not usually a standard requirement in OTA curriculum, however Daytona State College has taken on the initiative for students and health professionals to use HL obtained through multiple perspectives in order to investigate under-addressed issues and gaps in health care outcomes. The intent is to require undergraduate students to screen, design, and promote activities supporting HL in all clients, particularly seniors, immigrants, low-income groups, and ethnic minorities. These planned activities being incorporated into curriculum and fieldwork experiences will utilize resources like, the Health Literacy Expanded Model and National Action Plan for Health Literacy, as the conceptual frameworks to promote comprehension and application of HL. In turn, this will improve stakeholders’ understanding of health literacy and incorporate effective attributes of health literacy to health care organizations (Brach et al., 2012; CDC, 2018a; Weekes & Phillips, 2015; Zarcadoolas, Pleasant, & Greer, 2006). Supporting materials from the Florida Literacy Coalition, Institute of Medicine, and National Institutes of Health will also be used to address client-centered care with the overall goal of improving quality of service and reducing health disparities.
The Health Literacy Model includes four key domains, i.e. fundamental, scientific, civic, and cultural literacy (see Appendix). Fundamental literacy includes concepts of reading, writing, articulation, and numeracy (Zarcadoolas et al., 2007). Seniors may experience a decline in their levels of functional literacy associated with cognitive, linguistic, and visual deficits secondary to aging (Wolf, 2008). For example, advanced age may cause nonnative English language speakers to revert to communicating in their mother tongue. On the other hand, scientific literacy influences a client’s understanding of physical and natural sciences for basic comprehension of staging and progression of a disease process, like understanding tumor markers and the staging process in metastatic cancers or sliding-scale insulin therapy for managing diabetes, while civic literacy pertains to an individual’s ability to make informed decisions based on resources provided by government agencies and related public health sources (Mosley & Taylor, 2017). Client knowledge about new infections such as, COVID-19, Zika, and Ebola, and/or awareness of vaccines available for preventing diseases like, shingles and pneumonia, are salient for client participation in civic activities (Wolf, 2008). The influence of culture on client-practitioner interaction and communication of sensitive health information is a component of cultural literacy (Zarcadoolas et al., 2007). Cultural literacy includes the practitioner’s knowledge, beliefs, and values about the concept of disability as a sociocultural paradigm (Perry, 2012).
The hope is by incorporating both educating OTA students on health literacy and the use of the Health Literacy Expanded Model as a conceptual framework during fieldwork, it will serve as the foundation of customizing literacy improvement strategies in the populations that practitioners serve (Benavot, 2015). This model can guide the design of targeted HL improvement by encouraging practitioners to choose relevant assessments, simulated scenarios, case studies, and video-based vignettes that support understanding of multiliteracies as a social practice (Perry, 2012). Simulation, digital technologies, and innovative media support the development of HL educational materials for clients and facilitate the integration of arts into a curriculum that is predominantly science-driven (Lewis, 2018). Shared knowledge between students and practitioners about the barriers to HL approaches in medical settings will lead to more in-depth understanding of complex, under-conceptualized issues related to health equity and support skill acquisition for the 21st century learner (Benevot, 2015).
One of the most significant challenges in implementing HL interventions is most practitioners have limited time and extensive caseload demands, which impede their ability to administer assessments and designing activities specific to HL (Lambert et al., 2014; Slater, 2006). Individuals with disabilities may experience stress and stigma impeding their ability to communicate effectively with healthcare professionals, meaning health literacy is critical to client safety and can influence healthcare expenditure significantly (Brach et al., 2012). Therefore, strategies for effective client communication focused on improving HL are frequently underutilized, which negatively impacts the quality of care, so high performing healthcare organizations should incorporate trainings in organizational planning specifically related to health literacy for the purpose of quality assurance and improvement (Schwartzberg, Cowett, VanGeest, & Wolf, 2007; Turner et al., 2009; Weekes & Phillips, 2015). Academic programs must support artistic and creative endeavors in students to promote innovation in health literacy education.
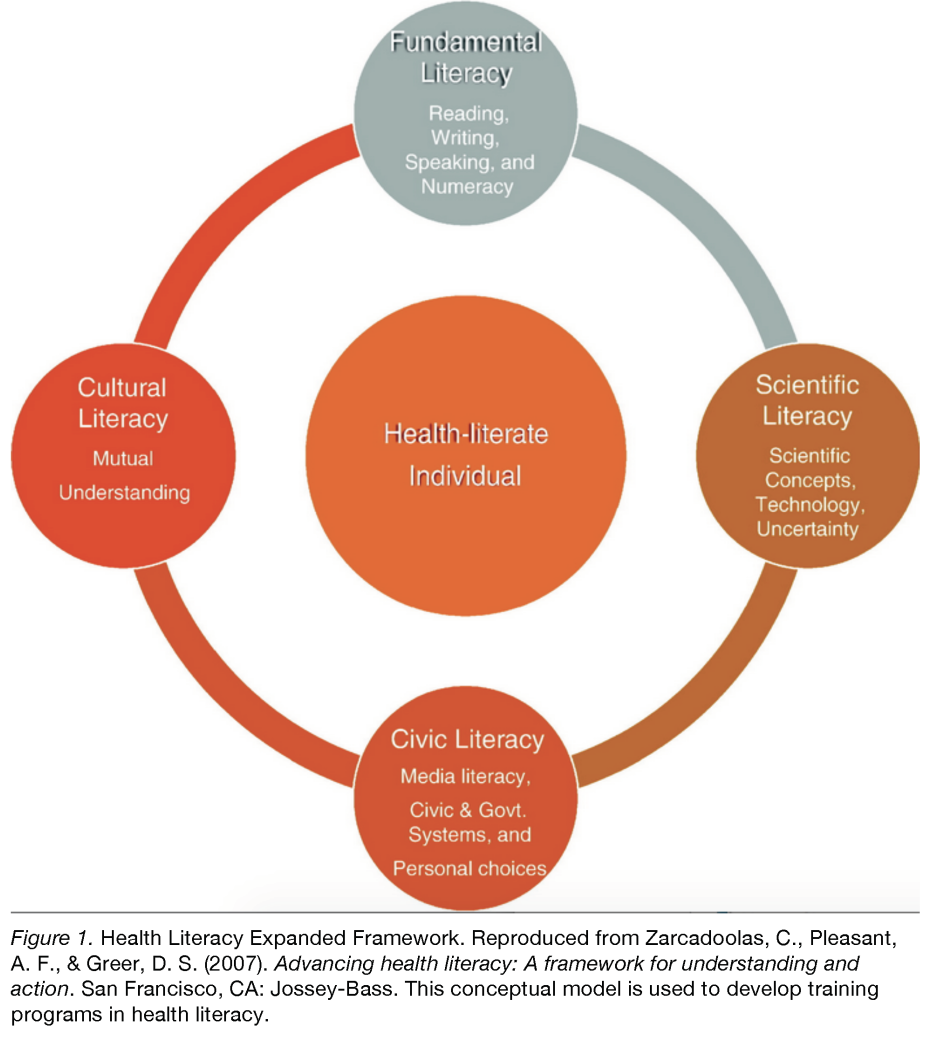
Occupational therapy assistant students can support practitioners and health care organization in multiple ways, including identifying signs of low literacy in clients, edit written materials for ease of comprehension, develop patient handouts with pictorial cues and inclusion of elementary concepts, and administer screenings, such as Health Literacy Assessment Questions and the Health Plan Organizational Assessment of Health Literacy Activities (Brach et al., 2012; DeWalt et al., 2010; Gazmarrian, Beditz, Pisano, & Carreon, 2010; Hadden, 2015). OTA students can then assist occupational therapy practitioners in facilitating the design and implementation of effective health literacy-based interventions through root-cause analyses of these assessments (Brach et al., 2012). In addition, future fieldwork placements, particularly during Level I fieldwork, may include assignments providing detailed description of HL assessments and suggested activities to support the various domains or multiliteracies described in the Health Literacy Expanded Model (Zarcadoolas et al., 2007).
In conclusion, the goal is local practitioners will be interested in exploring ways in which Daytona State College school can collaborate with field sites for HL-specific programming. Despite the constraints of high productivity and limited time available in health systems, such partnerships during experiential training can be instrumental in further shaping patient-centered care and supporting creative opportunities for HL-specific training.
References
Accreditation Council for Occupational Therapy Education [ACOTE]. (2018). 2018 ACOTE standards and interpretive guide. ACOTE Accreditation Standards. https://acoteonline.org/accreditationexplained/standards/ Benevot, A. (2015). Literacy in the 21st century: Towards a dynamic nexus of social relations. International Review of Education, 61, 273-294. doi:10.1007/ s11159-015-9463-3
Brach, C., Keller, D., Hernandez, L., Baur, C., Parker, R., Dreyer, B., … Schillinger, D. (2012). Ten attributes of health literate health care organizations. National Academy of Sciences. https://nam.edu/ wp-content/uploads/2015/06/BPH_Ten_ HLit_Attributes.pdf
Centers for Disease Control and Prevention [CDC]. (2018a). What is the national Action plan to improve health literacy? National Action Plan to Improve Health Literacy. https://www.cdc.gov/ healthliteracy/planact/national.html
Centers for Disease Control and Prevention [CDC]. (2018b). Health literacy. Older Adults.
https://www.cdc.gov/healthliteracy/ developmaterials/audiences/olderadults/ index.html#content
DeWalt, D. A., Callahan, L. F., Hawk, V. H., Boucksou, K. A., Hink, A., Rudd, R., & Brach, C. (2010). Health literacy universal precautions toolkit. Rockville, MD: Agency for Healthcare Research and Quality
Gant, A. (2013). Census: Volusia, Flagler aging faster than Florida. The Daytona Beach News-Journal. https://www.newsjournalonline.com/article/LK/20130612/ News/605067629/DN/
Gazmararian, J., Beditz, K., Pisano, S., Carreon, R. (2010). The development of health literacy assessment tool for health plans. Journal of Health Communication, 2, 93-101.doi:10.1080/10810730.2010 .499986.
Hadden, K. B. (2015). Health literacy training for health professions students. Patient Education and Counseling, 98(7), 918-920. doi:10.1016/j. pec.2015.03.016
Lambert, M., Luke, J., Downey, B., Crengle, S., Kelaher, M., Reid, S., & Smylie, J. (2014). Health literacy: Health professionals’ understandings and their perceptions of barriers that Indigenous patients encounter. BMC Health Services Research, 14, 614. doi:10.1186/ s12913-014-0614-1
Leu, D. J., Kinzer, C. K., Coiro, J., Castek, J., & Henry, L. A. (2017). New literacies: A dual-level theory of the changing nature of literacy, instruction, and assessment. Journal of Education, 197, 1–18. doi:10.1177/002205741719700202
Lewis, M. E. (2018). STEM and STEAM: 12 | FOCUS - SPRING ‘21 Importance of integration [Powerpoint Slides]. https:// blackboard.jhu.edu
Mosley, C. M., & Taylor, B. J. (2017). Integration of health literacy content into nursing curriculum utilizing the Health Literacy Expanded Model. Teaching and Learning in Nursing, 12(2), 109-116. doi:10.1016/j.teln.2016.12.005
National Network of Libraries of Medicine. (2011). Health literacy. https://nnlm.gov/priorities/topics/health-literacy Perry, K. H. (2012). What is literacy? - A critical overview of sociocultural perspectives. Journal of Language & Literacy Education, 8(1), 50–71. Retrieved from http://jolle.coe.uga. edu/wp-content/uploads/2012/06/What-is-Literacy_K
Perry.pdf Schwartzberg, J. G., Cowett, A., VanGeest, J., & Wolf, M. S. (2007). Communication techniques for patients with low health literacy: A survey of physicians, nurses, and pharmacists. American Journal of Health Behavior, 31(1), 96-104. doi: 10.5555/ajhb.2007.31.supp.S96 Slater, D. (2006). The ethics of productivity. OT Practice. American Occupational Therapy Association.
Turner, T., Cull, W., Bayldon, B., Klass, P., Sanders, L., Frintner, M., … Dreyer, B. (2009). Pediatricians and health literacy: Descriptive results from a national survey. Pediatrics, 124(3), 299-305. doi:10.1542/peds.2009-1162F.
Vernon, J. A., Trujillo, A., Rosenbaum, S., & DeBuono, B. (2007). Low health literacy: Implications for national health policy. Alabama Department of Public Health. https://www.alabamapublichealth.gov/alphtn/ assets/092017lowhealthliteracy.pdf
Weekes, C., & Phillips, T. (2015). A mile in my patient’s shoes: A health literacy simulation for baccalaureate nursing students. Clinical Simulation in Nursing, 11(11), 464-468. doi:10.1016/j. ecns.2015.09.001
Wolf, M. (2008). Proust and the squid: The story and science of the reading brain. New York, NY: Harper Collins.
Zarcadoolas, C., Pleasant, A. F., & Greer, D. S. (2007). Advancing health literacy: A framework for understanding and action. San Francisco, CA: Jossey-Bass.
